DO NOT LOVE AUTUMN? CHECK THE THYROID!
“Autumn time, charm eyes …” It seems that among the classics it was customary to
admire the fall. But which of us can confess our sincere love for
this time of year?
In the landscapes there is neither spring freshness, nor summer
revelry of colors, nor winter purity. There is little sun, a
lot of rain and slush . And the mood to match the weather – it is in the fall that many complain of
a breakdown, fatigue, drowsiness and general weakness.
However, you should not attribute the bad mood only to the weather – it
may well turn out to be a symptom of a dangerous disease.
The thyroid gland is a small organ, but it is an extremely important
element of the entire endocrine system. And if it is not in order, then the
whole organism suffers. The insidiousness of the thyroid gland is that
suspecting something is amiss is not so simple – the diseases do not have vivid
symptoms. And in the absence of adequate treatment, they are fraught with serious
complications. The thyroid gland uses iodine to produce
iodine-containing hormones that are involved in the regulation of metabolism,
which means they affect the body as a whole. Thyroid is naughty – and a
slender beauty will turn into an apathetic obese woman, and an energetic
young man – into a puffy neurotic. The good news is that
thyroid disease can be treated very well. It is only important to
recognize them in time .
Laboratory tests play a decisive role in identifying thyroid dysfunctions . You just need to
measure the level of certain hormones and antibodies in the blood. You can check
if everything is in order with the thyroid gland in the CityLab.
DIABETES: WHEN SUGAR DOESN’T MAKE LIFE SWEETER
According to the World Health Organization, in 2014, about 9% of the adult population of the planet suffered from it. Specialists note an increase in the incidence among children, which makes this problem even more relevant.
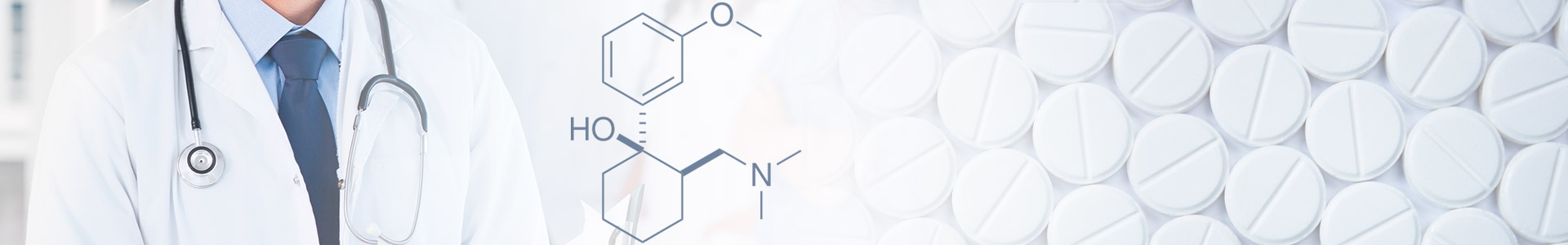
Diabetes is a disease of the endocrine system, in which there is an increased level of sugar in the blood due to a deficiency of insulin (the hormone that is responsible for the “processing” of glucose). Its lack can be absolute when it comes to problems with the insulin “factory” – the pancreas. Doctors in this case are diagnosed with type I diabetes. The second option: insulin is produced in sufficient quantities, but the mechanism of its interaction with cells is disrupted. Thus, insulin is enough, but it “does not work.” This condition is called insulin resistance. Until a certain point, the body by inertia continues the production of the hormone, but over time it decreases significantly. So in a very simplified form, you can describe the course of type II diabetes mellitus, which is the most common pathology.
The list of complications of this disease is very wide, and all of them are somehow related to excess glucose in the blood. The great Hippocrates made this diagnosis, tasting sugar in the urine of his patient. Fortunately, today laboratory diagnostics has stepped far forward. In the arsenal of doctors there are many types of studies that can speak with high confidence about the development of diabetes mellitus, and also allow you to track the dynamics of the pathological process. “CityLab” offers to use the comprehensive study “ Risk of Diabetes” , which includes all the diagnostically important tests necessary to suspect and detect the disease at an early stage:
The level of glucose in the blood is the starting point for the doctor in the process of differential diagnosis.
HBA1c (Glycated Hemoglobin) and fructosamine – will “tell” the doctor about the increased level of glucose in the body, even if a single measurement of fasting blood glucose is normal.
Determining the concentration of Insulin and the C-peptide (this is part of the insulin molecule) helps to evaluate the endocrine function of the pancreas.
Antibodies to β-cells of the pancreas and Antibodies to glutamate decarboxylase (GAD) – can “predict” the development of diabetes mellitus sometimes several years before it begins.
And if problems with glucose metabolism in the body have already begun, you need to remember that in the first place, eyes and kidneys are at risk. Therefore, it is important to visit an optometrist and regularly do a urine test:
Determination of albumin in urine is a diagnostic criterion for diabetic nephropathy (impaired renal function due to diabetes).
A blood glucose test can be called a classic in diagnosing diabetes. However, its results are not always clear. Glucose levels can vary depending on the general physical condition of a person, due to stress, individual characteristics of the body and after eating. This is why glucose is usually measured on an empty stomach. But in an empty stomach, glucose levels may be normal for some time after the process of glucose utilization in the body is already violated.
Determining the level of glycated hemoglobin HbA1c (a hemoglobin molecule associated with glucose) is devoid of these disadvantages – its concentration is not subject to daily and other fluctuations, does not depend on food intake. Therefore, this method is recognized by WHO as the “gold standard” in the diagnosis and control of diabetes. The life span of an erythrocyte (a blood element containing hemoglobin HbA1c) is 2-3 months. Thus, the doctor gets the opportunity to get information about the average glucose level in the body during this entire period.
Determining the level of fructosamine is a similar method in which the concentration of the products of the interaction of glucose with proteins is evaluated . It reflects the glucose content over the past 3 weeks. This parameter is most effective in the early stages of diabetes.